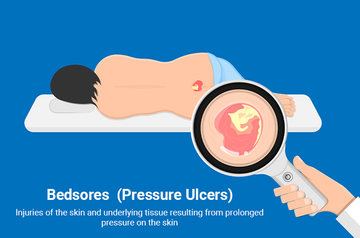
Why/How does Bedsore happen?
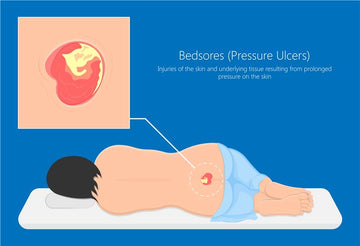
Pressure
Continuous pressure on the skin compresses tissues against bone or hard surfaces, reducing blood flow and causing tissue damage.
Friction
Friction is a big risk factor for bedsores, especially for those with limited mobility. Constant rubbing against sheets or clothing irritates and thins the skin, making it vulnerable. This weakens its defense against the pressure that ultimately causes bedsores.
Shear
Shearing happens when your skin stays stuck in one place, but your body slides down. This stretching and tearing can damage the tiny blood vessels under the skin. Without enough blood, the tissue gets weak and can turn into a bedsore.
Moisture
Excessive moisture softens the skin, making it more susceptible to damage and increasing the risk of infection.
Immobility
Limited mobility reduces the ability to change positions, increasing pressure on vulnerable areas.
Poor nutrition
Malnutrition weakens skin integrity and impairs tissue repair.
Medical conditions
Certain conditions, like diabetes or spinal cord injuries, increase the risk of bedsores by affecting blood flow and sensation.
Complications of bedsores
Infection
When the skin breaks down, it becomes susceptible to bacterial infection, which can lead to cellulitis (a bacterial skin infection), osteomyelitis (bone infection), or sepsis (a life-threatening infection that spreads through the bloodstream).
Cellulitis
This is a common bacterial skin infection that can occur when bacteria enter through a break in the skin, causing redness, swelling, and pain in the affected area.
Sepsis
In severe cases, an untreated bedsore can lead to sepsis, a life-threatening condition characterized by a systemic inflammatory response to infection. Sepsis can cause organ dysfunction and failure and requires prompt medical attention.
Deep Tissue Injury
Pressure ulcers can cause deep tissue damage, leading to pain, tissue death, and even sinus tracts (channels connecting to deeper tissues).
Contractures
Prolonged immobility due to bed rest can lead to contractures, where the muscles and tendons become shortened and stiff, resulting in limited joint mobility and function.
Loss of Function
Severe pressure ulcers can impair mobility and overall function, making it difficult for individuals to perform daily activities independently.
Stages of Pressure Ulcers:
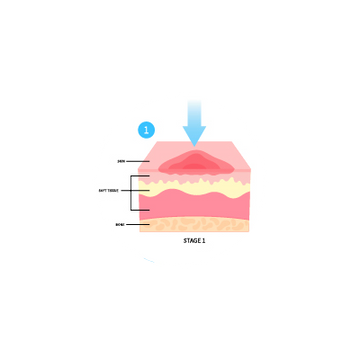
Stage 1
The skin is intact but may appear red or discolored. It may feel warm, firm, or soft compared to the surrounding skin. Stage 1 pressure ulcers do not blanch (turn white) when pressure is applied.

Stage 2
The skin breaks open, forming a shallow ulcer or abrasion. The ulcer may appear as a blister or shallow crater. It involves the epidermis (outer layer of skin) and may extend into the dermis (deeper layer of skin).
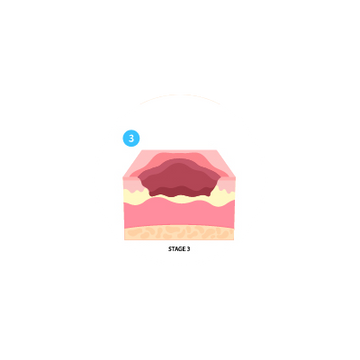
Stage 3
The ulcer extends deeper into the skin, affecting the subcutaneous tissue (fat layer) and creating a deep crater. The ulcer may have a foul odor and show signs of infection.
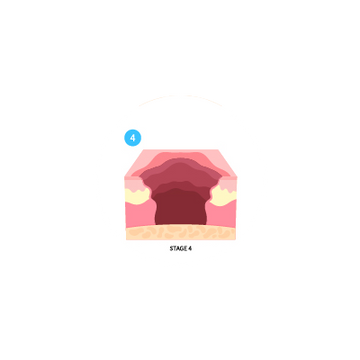
Stage 4
This is the most severe stage, where the ulcer extends through all layers of the skin, including muscle, tendon, and possibly bone. There may be extensive tissue damage and necrosis.