How should I identify if my patient is prone to bedsore (who is prone to developing bedsores)
Immobility
Patients who are bedridden or have limited mobility are at a higher risk. They are unable to shift their weight, leading to prolonged pressure on certain areas of the body.
Poor Circulation
Conditions such as diabetes or cardiovascular diseases can impair blood flow, increasing the risk of tissue damage.
Decreased Sensation
Patients with neurological disorders or spinal cord injuries may have reduced sensation, making them less aware of pressure and friction on their skin.
Poor Nutrition
Malnourished individuals lack the nutrients necessary for tissue repair and maintenance, making their skin more susceptible to breakdown.
Advanced Age
Elderly patients often have thinner skin, decreased elasticity, and reduced tissue resilience, making them more prone to skin breakdown.
Incontinence
Exposure to moisture from urine or feces can weaken the skin's integrity, increasing the risk of bedsores.
Friction and Shear
Patients who are frequently moved or repositioned improperly can experience friction and shear forces, which can damage the skin's deeper layers.
History of Pressure Ulcers
Patients who have previously experienced bedsores are more likely to develop them again, especially if preventive measures are not implemented.
Skin Condition
Assess the patient's skin for signs of redness, warmth, or discoloration, particularly over bony prominences such as the sacrum, heels, elbows, and hips.
Pain or Discomfort
While pain can be a symptom of existing bedsores, it can also indicate areas of pressure or tissue damage before visible signs appear.
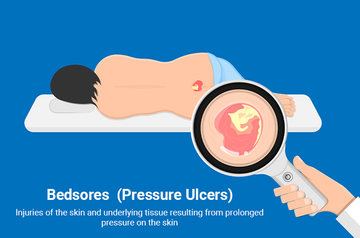
What should I look for to identify bedsores?

1. Changes in Skin Color
Look for patches of skin that are red, blue, purple, or black. Discoloration may indicate tissue damage.
2. Changes in Skin Texture
The affected area may feel unusually firm, soft, or spongy compared to the surrounding skin.
3. Pain or Tenderness
The person may complain of pain or discomfort in specific areas, even if there's no visible damage yet.
4. Swelling
Swelling may occur in the area where the skin is affected.
5. Warmth or Coolness
The skin around the affected area may feel warmer or cooler than the surrounding skin.
6. Blisters or Sores
Look for open wounds, blisters, or sores, especially in areas where the bone is close to the skin, like the heels, ankles, hips, and tailbone.
7. Localized Area
Bedsores often develop over bony prominences like the back of the head, shoulders, elbows, lower back, buttocks, hips, and heels.
8. Lack of Sensation
In some cases, the person may have reduced sensation in the affected area due to nerve damage, making it harder for them to feel discomfort until the sore has developed significantly.
What should we do to prevent bedsores?
Use Soreze Gel and Soreze Spray
Prevent bedsores by using skin protectant products like Soreze Gel and Soreze Spray. Our products are dermatologically tested and clinically proven to help shield your elderly loved one's skin from the friction and moisture that can lead to Pressure Sores.
Soreze Gel forms a water-repellent barrier film that lasts for hours, even with sweat or incontinence.
Soreze Spray offers a similar benefit with a convenient, no-touch application. Remember, these products are for the prevention on unbroken skin, so consult a healthcare professional if your loved one already has a bedsore.
Regular Positioning
Encourage the individual to change their position frequently, at least every two hours if possible. This helps to relieve pressure on specific areas of the body.
Use of Support Surfaces
Invest in specialized support surfaces such as mattresses, cushions, or overlays designed to distribute pressure evenly and reduce the risk of bedsores.
Maintain Skin Hygiene
Keep the skin clean and dry, and use moisturizers to prevent dryness and cracking, which can make the skin more susceptible to damage.
Nutrition
Ensure the individual receives a well-balanced diet with adequate protein, vitamins, and minerals, as nutrition plays a significant role in maintaining skin health.
Stay Active
Encourage gentle exercises or range of motion activities to improve circulation and muscle strength, which can help prevent pressure ulcers.
Inspect Skin Regularly
Check the skin for any signs of redness, irritation, or breakdown, especially in areas prone to pressure ulcers such as the heels, elbows, sacrum, and hips.
Provide Proper Support
Use pillows or foam wedges to support bony prominences and keep them from directly contacting surfaces for extended periods
Manage Moisture
Keep the skin clean and dry, and use moisture-absorbing products or barrier creams to protect against moisture-related skin damage.
Avoid Friction and Shear
Minimize friction and shear forces on the skin by using proper lifting and transferring techniques, as well as avoiding dragging or pulling the individual across surfaces.
Regular Monitoring
Continuously assess the individual's risk for developing bedsores and adjust preventive measures accordingly, especially if there are changes in their health status or mobility.
What should a person do if a bedsore develops?
Use Soreze Advance Gel
Soreze Advance Gel effectively treats bedsores and provides relief. Its formula promotes healing and soothes discomfort. By using it as directed, you can actively support skin recovery. This specialized gel offers both treatment and relief for those with bedsores.
Relieve pressure
Remove pressure from the affected area by repositioning the individual regularly. Use pillows, foam pads, or specialized cushions to distribute pressure evenly and reduce friction.
Keep the area clean and dry
Clean the affected area with mild soap and water, and gently pat it dry. Avoid rubbing the skin, as it can cause further irritation.
Apply appropriate dressings
Depending on the severity of the bedsore, your healthcare provider may recommend specific dressings or topical treatments to promote healing and prevent infection.
Optimize nutrition
Ensure the person is receiving adequate nutrition, including protein, vitamins, and minerals, to support tissue repair and overall health.
Monitor for signs of infection
Watch for signs of infection such as increased redness, warmth, swelling, or drainage from the sore. If you notice any of these symptoms, seek medical attention promptly.
Consult a healthcare professional
If a bedsore develops or if you're unsure how to care for it properly, consult a healthcare professional. They can assess the severity of the sore and recommend appropriate treatment options
How should a person manage a bedsore patient?
Wound Care
Follow healthcare provider instructions for dressing changes and wound care. This may involve cleaning the wound with saline solution, applying prescribed topical treatments or ointments, such as Soreze Advance Gel for treating existing Bedsores and providing relief, and using appropriate dressings to promote healing and prevent infection.
Nutrition
Ensure the patient is receiving adequate nutrition to support wound healing. A diet rich in protein, vitamins (especially A and C), and minerals like zinc is essential. Consult a registered dietitian for personalized dietary advice.
Hygiene
Keep the skin clean and dry. Regularly bathe the patient with mild soap and water, and gently pat the skin dry rather than rubbing. Moisturize the skin to prevent dryness, but avoid moisturizers near the wound site.
Re-positioning
Regularly change the patient's position to relieve pressure on vulnerable areas and prevent new bedsores from forming. Use pillows, foam pads, or specialized support surfaces to redistribute pressure and support proper body alignment.
Skin Assessment
Conduct regular skin assessments to identify early signs of pressure ulcers or changes in existing ones. Pay close attention to areas prone to pressure such as the heels, elbows, hips, and sacrum. To help prevent pressure ulcers, consider using Soreze Gel, a dermatologically tested and clinically proven gel that forms a protective barrier on the skin. Additionally, Soreze Spray offers a convenient option to prevent bed sores and diaper rashes with its easy application and long-lasting protection. Remember, prevention is key!
Mobility and Activity
Encourage mobility and regular movement within the patient's capabilities. Even small changes in position can help relieve pressure on vulnerable areas. Physical therapy may be beneficial for maintaining mobility and strength.
Support Surfaces
Invest in pressure-relieving support surfaces such as specialized mattresses, cushions, or overlays designed to reduce pressure and shear forces on the skin.
Education
Educate the patient, caregivers, and family members about the importance of proper skincare, nutrition, and pressure ulcer prevention techniques. Guide how to recognize early signs of skin breakdown and when to seek medical attention.
Collaboration
Work closely with a multidisciplinary healthcare team including nurses, physicians, dietitians, and wound care specialists to develop and implement an effective management plan tailored to the patient's specific needs.
Monitor and Adjust
Continuously monitor the patient's progress and adjust the management plan as needed based on the response to treatment, changes in the patient's condition, and any new developments or challenges that arise.